Trigger Points are “KNOT” Fun

Bracing for Pain
November 21, 2022
Importance of Vitamin D During Winter Months and Depression
November 30, 2022Trigger Points- “Knot” Fun
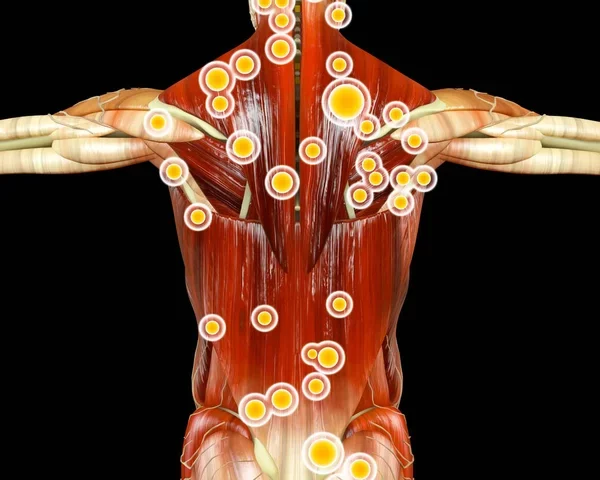
Have you ever been told the cause of your pain is due to a trigger point when having a massage or visiting a chiropractor? A very common response is – what’s that? Trigger points are casually referred to as “knots”. Myofascial trigger points are rope-like sensitive, knotted bands of muscle fibers and surrounding fascia that have been stuck in a contracted state. A more technical definition is focal points of muscular dysfunction that involve contracted sarcomeres and an associated localized myofascial energy crisis that allows for prolonged actin-myosin cross linkage mainly in the center of the muscle belly where the motor endplate enters. Woof.
Trigger points are the result of muscular injuries, strains, or trauma where muscle fibers, fascia, ligaments, and tendons have become weakened, overstretched, or inflamed which causes tiny tears. As the body and tissue heals, these fibers become knotted which restricts fresh blood supply to the injured site. Frequently, the affected muscle fibers shorten to protect itself from further injury. They can result from acute trauma like a car accident or repetitive microtrauma and overuse. Other contributing factors include poor nutrition, mental/emotional stress, structural imbalances, and faulty movement patterns. Muscles that have had a previous surgery are prone to developing trigger points as well as the muscles surrounding joints.
Myofascial trigger points are quite common, in fact 85% of people experience a trigger point at some time. This makes sense when considering our skeletal muscle collectively is one of the largest organs which represents approximately 40% of total body weight and most sources report over 600 individual muscles- any of which can develop a myofascial trigger point. Trigger points affect our movement patterns due to the shortening and stiffening which decrease range of motion, increase muscle fatigue, and decrease recovery. They can also cause spasms of other nearby muscles. Muscles that contain a trigger point will contract excessively when in use and can even partially disarticulate joint motion causing a catch or pop. Movement of any joint requires some muscles to contract while others relax, and trigger points can restrict either. This results in pain and discourages full range of movement.
Trigger points can also be active or latent. Active trigger points cause pain at rest and refer pain to other regions when compressed or being worked on. Latent trigger points typically do not have resting pain or referral patterns but can cause restricted movement or weakness and tenderness to compression. Referred pain from trigger points do not follow typical dermatone or nerve root distributions. Sub-occipital and upper trapezius trigger points, for example, refer pain to the skull causing headaches while the piriformis muscle contributes to sciatica. Other common muscles prone to trigger points include the masseter, temporalis, levator scapulae, sternocleidomastoid, glute medius, hamstrings, and calf muscles. CT scans, MRIs, and x-rays are unreliable for diagnosing trigger points and are found through physical exam and palpation.
There are a variety of treatments for myofascial trigger points. Manual therapy from a massage therapist, chiropractor, or physical therapist are some of the most common treatment methods. Difficult, severe, or nonresponsive trigger points can also be treated by medication via trigger point injections. There are, however, some possible at-home techniques available to avoid enlisting the help of a healthcare professional. Gentle stretching after exercise or activity paired with self-massage can be very helpful. Self-massage can be done with numerous tools including a foam roller, tennis ball, ‘thera-cane’/ ‘back-nobber’ as well as other self-release tools on the market. Even relatives or friends can be of assistance with simple digital pressure placed into a trigger point. Using moderate pressure, hold for 5-7 seconds and quickly release the pressure. Repeat this 3-5 times and can be done every other day. Placing pressure directly over the trigger point induces ischemia (blood flows away) followed by release and reactive vasodilation (blood flow returns) with hopes of forcing muscle relaxation. It should also be noted that engaging in an active treatment plan focused on postural correction and muscular imbalance with exercise is most optimal in combination with some of these passive treatment methods.
—
This article was written by Dr. Deryk Harting, one of the members of Chambers Medical Group’s team of car accident chiropractors who offer a variety of treatments and therapies ranging from diagnostic testing to various soft tissue therapies for car accidents and injuries in Kentucky.
If you or somebody you know has been in a car accident, be sure that you seek medical attention from a car accident doctor or car accident chiropractor to treat your injuries. Visit Chambers Medical Group to receive world-class medical treatment for your injuries.
Chambers Medical Group has car accident medical clinics in the following locations:
- Car Accident Medical Clinic in Tampa
- Car Accident Medical Clinic in Plant City
- Car Accident Medical Clinic in Brandon
- Car Accident Medical Clinic in Lakeland
- Car Accident Medical Clinic in Sarasota
- Car Accident Medical Clinic in Louisville
- Car Accident Medical Clinic in Lexington
- Car Accident Medical Clinic in Florence